The Denial and Appeals Process in Medical Billing
Medical coders and billers both work with clinical staff and must know medical terminology, anatomy, and pathophysiology to understand physician notes and operative reports. Medical coders sometimes participate in the billing process and may code for billing companies. In small physician practices, it’s not uncommon for the same person to serve as medical coder and medical biller.
- If you still have questions about this process and how it would apply to your clinic, give us a call to ask your questions.
- The Division of Energy Employees occupational Illness Compensation (DEEOIC) will not dictate what option an employee must accept, nor will decisions be made based solely upon cost.
- A strong billing system needs the billers to stay on top of claims status and know how a denial can be recovered through appeals.
- This article will take you through the appeals process in medical billing and the key aspects you need to keep in mind to maximize the revenue flow in your organization.
- For example, the provider may have used the wrong codes or failed to include all of the necessary documentation.
In some cases, denials may be the result of a payer’s policy or guideline. For example, a payer may have a policy that limits the number of physical therapy sessions that are covered per year. In these cases, providers can appeal the denial by providing evidence that the additional sessions are medically necessary.
Forms for requesting a second look should be used
You’ll most likely get the mailing and any electronic sending addresses from the company’s website when you get your insurance-specific forms. You may see it on the EOB, but be sure that is actually the correct address for sending appeals. You don’t want to do all the necessary paperwork to have nothing come of it. With Denials Management workflow tools, you can automate forms and data fields in Rivet so you can reduce error and manual data entry. Keep continuous record of instructions, payer policies and payer contact info by payer and denial type.
When a payer denies a claim, the remittance advice provides billing staff with a denial code(s) and a brief explanation as to why the claim was denied. The denied claim should be reviewed by the billing staff to determine whether additional information is needed, if errors need to be corrected, or if the denial should be appealed. At the core of the medical bill reimbursement process is the use of treatment suites. The treatment suites used by the DEEOIC are contained in a database maintained by medical professionals within the OWCP.
The Appeals Process in Medical Billing
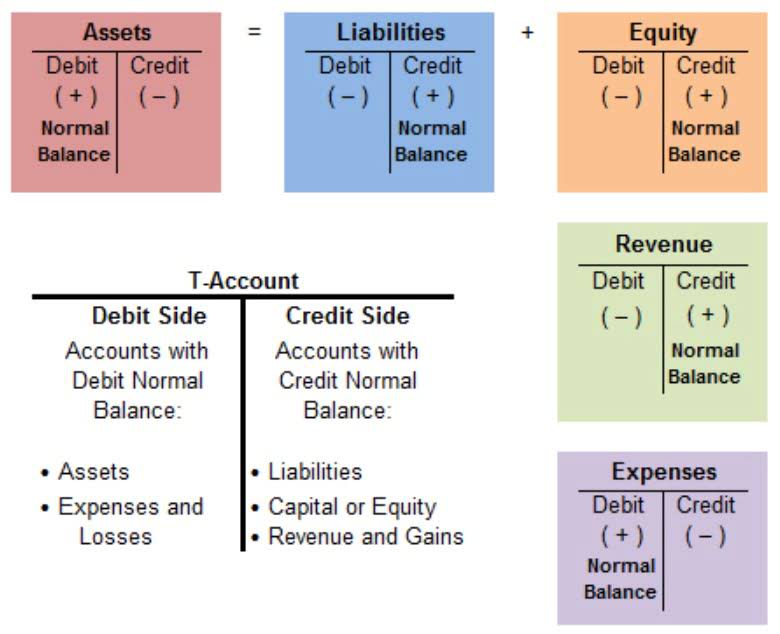
The use of medical codes helps summarize medical services and reports. These medical code sets help medical coders document the patient conditions and describe the healthcare procedure(s) performed to treat their conditions. A successful medical billing team requires the capacity and process for following up on claims.
So you got a huge bill, and you’re sure there’s been a mistake, either in the bill or the insurer’s processing of a claim. We cannot guarantee that you will win, but at least you will have tried. Sometimes we can, though arguing bills is not our core business — we love to tell people how to avoid bad bills on the front end if they can. Credit will not be awarded for educational activities completed prior to certification. Make sure you document all phone conversations in the patient system or billing software. Note who you spoke with, what the agreement was, and the reference number (get this number from the provider representative; it documents the conversation on the payer’s end).
What is the difference between CPB Medical Billing course and the CPC Preparation course?
When the accepted condition(s) are coded and billed with the correct ICD-9/10 Code, the volume of suspended and denied bills is significantly reduced. Consequently, accurate code selection expedites provider reimbursement for all approved medical services rendered to the claimant. The Certified Professional Biller (CPB™) certification prepares medical billers with the technical knowledge and skills to maintain all aspects of the revenue cycle. Without deep knowledge and expertise in medical billing and the unique understanding of insurance requirements, provider reimbursement may be denied, delayed, or incomplete. Grants will be made available to support States’ efforts to establish or strengthen consumer assistance programs that provide direct services to consumers with questions or concerns regarding their health insurance.
The appeals process in medical billing shields the providers from unnecessary revenue loss. Here are the answers to some top frequently asked questions that you should know. Front-end medical billing staff should be well versed in their organization’s payer mix. Errors occurring at any stage in the billing cycle can prove costly in terms of revenue and administrative workload, which underscores the value of medical billers able to command their role in the billing process. The financial health of physician practices and provider organizations, such as hospitals, health systems, and surgery centers depends on the effectiveness of front-end and back-end billing staff. While the medical billing cycle comprises numerous steps that can take anywhere from a few days to several months, accurate billing and timely follow-up are No. 1 priorities.
This career path has afforded me the ability to provide well for my family and have flexibility to work at home when I want. This is a field where the education is endless—you learn something new every day—and the friendships are endless. I’ve found a job I love and haven’t worked a day in my life.
However, the system will allow entry of an ICD-9 if appropriate. Ultimately, the medical eligibility begin date is the driving factor on whether an ICD-9 or ICD-10 code must be used on a medical condition. If the medical eligibility begin date is on or after October 1, 2015, the ICD-10 code is what will be reflected throughout the system wherever ICDs are reflected. CEs will also reference ICD-10 in decisions and development letters if the filing/eligibility begin date is on or after October 1, 2015. The MBPU reviews all submissions submitted to the medical bill inquiries mailbox and it determines the proper course of action. As noted above, the MBPU reviews and answers all policy, treatment suite, and medical provider outreach questions.
Relationships between MACs and Functional Contractors
The best way to fight your cause is to support your appeal with the necessary documentation. Stay informed about our product updates, events and latest trends in patient access, mid cycle and backend revenue cycle management. In addition to regular communications through statements and availability to answer questions, patient follow-up can involve offering conveniences to accelerate collections and lessen bad debt. These conveniences might include payment plans and online payment methods. Once these final payments are made by patients, commonly arriving by mail, they should be posted and balanced. With many patient cases, this completes the billing process and closes the patient account.
- You’ll learn everything you need to prepare for the CPC and CPB certification exams.
- When the accepted condition(s) are coded and billed with the correct ICD-9/10 Code, the volume of suspended and denied bills is significantly reduced.
- In these cases, providers can appeal the denial by submitting additional documentation, such as medical records or letters from physicians, to support the medical necessity of the service.
- Front-end medical billing staff should be well versed in their organization’s payer mix.
- If the medical eligibility begin date is on or after October 1, 2015, the ICD-10 code is what will be reflected throughout the system wherever ICDs are reflected.
- In these cases, providers can appeal the denial by correcting the errors and resubmitting the claim.
- We hope that before the event or procedure you asked “How much will this cost? How much will it cost me? What if I paid cash?” Our handbook about that is Part 1 of this series.
Invoices are sent to patients when required and payments are posted and reconciled. But much more happens before, after, and between in the medical biller’s workday. For all medical conditions with a medical eligibility medical billing process begin date on or after October 1, 2015, the CE will use ICD-10-CM coding in ECS, development, and decisions. If the condition is input into ECS after October 1, 2015, ECS will default to entry of an ICD-10 code.


Leave a Reply